Introduction:
Sickle Cell Disease (SCD) affects nearly 100,000 people in the United States (Centers for Disease Control and Prevention, 2023). Vaso-occlusive episode (VOE) is the most common reason for hospitalization in SCD. Many providers are unfamiliar with the pain management timing and dosages required to adequately treat these episodes (Jang et al., J Transl Med 2021). Nationally, areas with comprehensive sickle cell centers have shown decreased hospital utilization, fewer VOEs, and improved quality of life (Oyedeji et al. JAMA 2020). Even in areas without a comprehensive center, implementing individualized pain care plans for SCD has reduced admission rates of high-utilizing patients while not impacting their pain rating scores (Welch-Coltrane et al. Pain Medicine 2021).
Our academic hospital, Oregon Health and Science University (OHSU), lacks a comprehensive SCD center and VOE treatment plans are not easily accessible for these patients. We conducted a retrospective analysis on a cohort of patients with SCD to investigate the factors influencing the length of emergency department (ED) and hospital stays for VOE. We aim to identify if implementing individualized pain plans via a standardized template within the electronic health record (EHR) for these patients will decrease hospital admission, length of stay and time to ED discharge. We also aim to integrate individualized pain plans into the EHR that would allow for direct exposure to the care team by creating plans that are easily accessible, reviewed, and routinely utilized for clinical decision-making.
Methods:
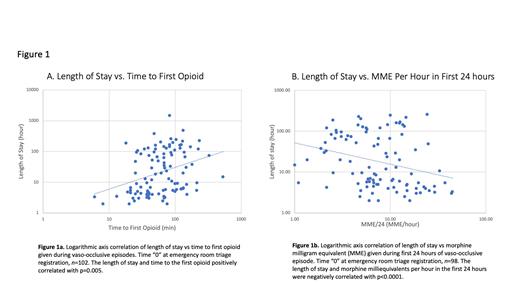
We performed a preliminary retrospective analysis of encounters (n=107) from 2008-2023 at OHSU, where the primary diagnosis was either a VOE or an equivalent diagnosis. Based on data demonstrating earlier maximum opioid doses leading to shortened hospital stays in frequent pain patients, we recorded the timing of the first opioid and morphine milliequivalents per hour in the first 24 hours (Payne et al. Pediatr Blood Cancer 2018). Additionally, we recorded the length of stay, admission rates, time to first IV fluid, and the type of IV fluid used. We performed a linear regression analysis on the collected data with the dependent variable as the length of stay across the independent variables of time to first opioid, time to first intravenous fluid, and morphine milliequivalents per hour during the first 24 hours after presentation.
Results:
Eighteen patients accounted for the 107 analyzed encounters. Thirteen patients (72%) had Hgb-SS disease, 2 (11%) had Hgb-SC disease, and 3 (17%) had Hgb-S-beta thalassemia. Sixty-two admissions (58%) were ED discharges, and 45 (42%) were ED to hospital admissions. The length of stay and time to the first opioid positively correlated with p=0.005 (Figure 1a). The length of stay and time to first intravenous fluid administration was also positively correlated with p=0.01. The length of stay and morphine milliequivalents per hour in the first 24 hours were negatively correlated with p<0.0001 (Figure 1b).
Conclusions:
Longer time to administration of opioids and intravenous fluids correlated with a longer length of stay in both the ED and the hospital. Additionally, lower morphine milliequivalents in the first 24 hours of presentation were associated with a prolonged hospital stay at our institution. We hypothesize that these three factors are secondary to delays in care and inappropriate initial treatment of VOE. To address these factors, we aim to implement standardized pain plans in the EHR of our institution. Implementation of individualized pain plans, particularly in the ED, has led to the earlier initiation of opioids (Della-Moretta et al. Ann Emerg Med 2020). We anticipate similar effectiveness for timely and appropriate fluid administration and adequate opioid dosing. We plan to continue retrospective analysis and compare this data to VOE encounters post-implementation. By implementing individualized plans that are integrated within the EHR and efficiently utilized by the care team, we hope to improve VOE management at our institution with decreased length of stay, less ED to hospital admissions, and improved patient satisfaction.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal